Publications IPH Magazine Special: 60th Anniversary Acoustic Comfort In Healthcare Environments: Music, Landscape And Cladding Material As Humanizing Solutions
- EDITORIAL
- Future Trends in Teaching and Research Hospital Design
- Jarbas Karman and the Hospital Architecture
- Surgical Centers: An Approach
- Acoustic Comfort In Healthcare Environments: Music, Landscape And Cladding Material As Humanizing Solutions
- Hospital Engineering and Maintenance: Committing To Maintaining Lives
- Communication and Leadership in Health Institutions
- The Relationship Between Professionals And Patients In The Health Sector - Tendencies And Perspectives
Acoustic Comfort In Healthcare Environments: Music, Landscape And Cladding Material As Humanizing Solutions
Fábio Bitencourt




Other alternatives and measurements to reduce the level of noise inside ICUs and other hospital environments can be used with the following strategies:
The cladding material for the ceiling can play an important role in the quality of acoustic comfort in healthcare facilities. They can be fixed or removable and for each one of them there are factors to be considered concerning its contribution for noise reduction. Regardless of how critical the environment is in relation to the possibility of transmitting disease (critical, semi-critical and non-critical) it must be taken into consideration the function of preventing and controlling infection based on the asepsis and cleaning recommendations, because according to the RDC number 50 "the appropriate cladding material for walls, floors and ceilings in critical and semi-critical areas must be resistant to washing and use of disinfectant" (BRASIL, 2002, p. 107).
Introduction
Buildings that hold health services are frequently assaulted by critical and stressful situations, which include interpersonal relationships and individuals with a certain degree of either physical or psychological distress. Therefore the environmental factors that define comfort (acoustic, visual, hygrothermal and ergonomic) play a crucial role throughout the process of architectural design.
The present work is a bibliographic narrative review aiming to describing and discussing the issues concerning acoustic comfort, entailing it to the architectonic responsibilities of the project that may allow better assistance outcomes for the health services (ROTHER, 2007; POPE, 2005). We highlight the conceptual aspects of the noise and the constant health hazards, the usage of landscape, music and cladding material and its applicability to the architectonic project, considering the risks and loss to health that justify them as essential factors to human comfort.
The hospital environment works in a paradox situation of being a place demanding special conditions of acoustic comfort with noise levels that respect recommendations established by technical standards and on the other hand also being a place with components and equipment that produce extremely noisy conditions.
It's a constant functional dilemma with several demands and solutions surrounded by multiple physical and functional aspects.
Intellectual activities and therapeutic procedures have processes that require concentration to be applied and, therefore, noisy environments may interfere directly in the quality of the diagnosis and the therapeutic processes. There are technical reasons and aspects of human health that justify the relevance of the contemporary concern in the matter.
1 Development
1.1 Conceptual and design references
The architect and engineer Jarbas Karman, who wrote and researched about the issue concerning the hospital environment, considered that among the "vicious of inception" from building health facilities, the noises and the vibrations leave few alternatives for afterward solutions for maintenance and safety. He characterizes the locations, building and special equipments of hospital facilities as "noisy gathering" that requires specific implementation with appropriate location delimitation (KARMAN, 2011, p. 78).

Picture 1 - Florence Nightingale sees patients at Scutari Militar Hospital, 1854. Source: Wellcome Library, V0004315.
According to the Anglo-Italian nurse Florence Nightingale, author of Notes on Hospital, published in 1856, the issue concerning patient therapeutic care was closely linked to the quality of the environment. Aspects concerning zenithal illumination and bed disposition in order to benefit from natural ventilation and acoustic protection would be a part of the assistance. Florence believes that the "unnecessary noise is the most cruel lack of care" (Apud HOSKING, 1999, p.163).
Some researches on "noise control in hospitals" in institutions in England published by the King's Fund Report show that in order to accomplish acoustic comfort "the most import fact to be controlled is the discipline over the health professional teams"(HOSKING, 1999, p. 163/4). Campaigns to attenuate the noises in health environments happen often and should be encouraged and not interrupted, as shown in pictures 2 to 6.

Picture 2 - A poster that brings the topic "Noise control in hospitals", in a campaign against noises developed by "Fougasse" (Cyril KenethBird) for the King's Fund.
Source: Hosking, 1999, p. 164.
The noise-related issues that are consequence of the concept of the project and the hospital building construction may establish the existence of complex solutions or most of the times "another sick hospital", according to Karman and his assessments on the hospital vicious inception (KARMAN, 2011, p. 79).
Understanding acoustic comfort means to comprehend and differentiate noise and its impacts on health, safety and well-being. Several authors use a more conventional concept to define the noise as an "undesirable sound" or "unpleasant sound" (NORD, 2012; BITENCOURT, 2011; IIDA, 2005; SOUZA, 2003; DOMENÈCH, 2002; BERNASCONI, 2001; GRANDJEAN, 1998).
According to German acoustic researcher and studious W. Hawell, "the sound is inconvenient when the target person doesn't see it as agreeing to his or her momentary interests" (GRANDJEAN, 1998, p. 263) and, therefore, can be classified as noise or undesirable sound. Or yet, according to a definition presented by professor Itiro Iida, "the noise is an auditory encouragement that doesn't bring useful information for the task in matter." (2005, p. 239).
Pictures 3, 4, 5 and 6 - Poster references from silence campaigns in hospitals. Source:
http://ihm.nlm.nih.gov (1943), 2014; HNSC, 2012.
Tolerance to noise is usually lower during a period of sickness and "demanding silence in hospitals is one of the oldest traditions in patient care" (HOSKING, 1999, p.163). Hence, controlling noises must be an important strategy of quality and comfort for all users (health professionals, patients and visitors), since noises are always connected to a relevant source of stress.
1.2 Noise, a danger to health
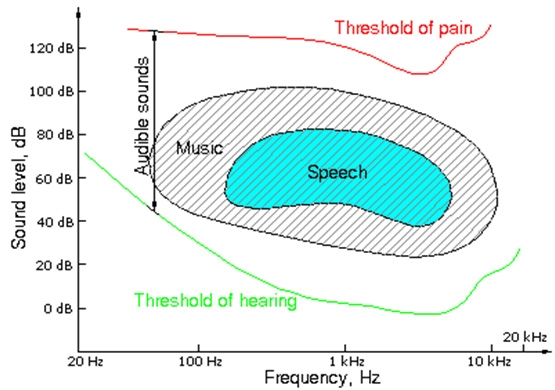
Understanding the phenomenon of the sound and how it propagates is essential to establish the appropriate barriers and protection systems needed to the acoustic quality necessary for human well-being.
The sound intensity level (SIL) is defined by the power of the sound and it's expressed in decibel (dB) in a curve A that reflects the closest to the human hearing and should be expressed in dB(A). The sound wave unities measured in a determined scale of time are defined as sound frequencies and expressed in Hertz (Hz) (ABRAHÃO, 2009; IIDA, 2005; SOUZA, 2003; GRANDJEAN, 1998).
To better understand the acoustic impact in environments where health care services take place it's fundamental to understand the concept of noises generated by interfering sound sources. Such noises are defined by the Norma Técnica Brasileira - NBR 12179, as "an aloof or temporary incident concerning the most characteristic purpose of the location in which the ambience sound is being assessed" (2003, p. 2). Considering that any noise originated from an aloof or temporary incident may impact the quality of the human comfort of those using health service facilities, they must be inserted when characterizing the noise to be considered, measured and effectively included in the acoustic assessment in order to control it.
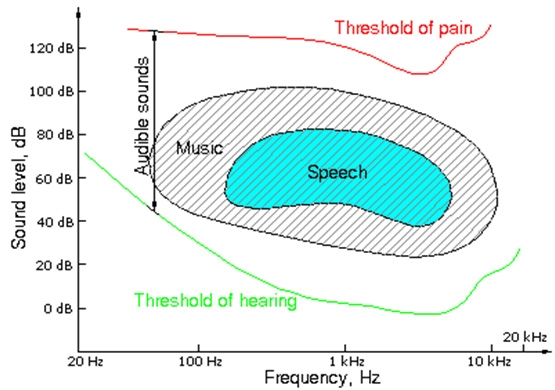
Picture 7 - Hearing and pain threshold in relation to the sound intensity level (dB [A]) and the sound frequency (Hz). Source: WOODSON, 1992.
At the same time, the relevance of the noise impact over activities undertaken in facilities for health assistance, for being usually recurring, highlights the need to be considered as obstacles for human acoustic comfort. Telephone and mobile sound signals, the noises from the nurse strollers, the conversations among health professionals, the sound signal from monitors, as well as other sounds produced by medical and hospital equipments must be considered as part of the noises collection produced inside healthcare buildings (SOUZA, 2003; BERNASCONI, 2001).
With effect, by analyzing the noises identified as inherent to the environment and the accomplishment of the functional activities, is possible that such sounds are inherent and not an interference, or an interference sound source as defined by NBR 12179 (ABNT, 1992).
In healthcare buildings and specifically in obstetric centers the activities inherent to the act of labour lead women to produce sounds, moan and scream due to the great amount of pain originated from the delivery. These noises generate levels of sound pressure that may be unpleasant to health professionals responsible for the obstetric procedures. The Sound Pressure Level (PA) can be explained as the representation of the measurement of pressure oscillations that move through a certain frequency and intensity range and that can be perceived by the human ear or according to the Iida (1997, p.240) the "intensity of a sound sensation".
According doctor and professor J. C. Yoder, from Pritzker School of Medicine from the University of Chicago, the noises produced in hospital environments can be a danger for the patients. He recommends that "hospitals should implement interventions to reduce the night noises in an effort to promote the patient's satisfaction and recovery, since reducing noises can be a simple way to adopt sensible habits" (YODER, 2012, p.1). Some procedures recommended in his work take nursing through the following actions:
- Ask patients about the best timeliness to proceed with personal hygiene and habits;
- Keep doors closed and reduced light in the circulation area with just enough intensity to proceed with night activities;
- Recommend less group talk in the circulation area.
1.3 The landscape and the silence
Landscape solutions can be an important alternative when approaching care as prevention, control and reduction of noises. When implemented in places with periphery urbanization that become noisy after the hospital was built the landscape solutions may present positive results softening the sound of the traffic as well as improving the environment and making the ambience more humanized (NORD, 2012, 2009; ULRICH, 2001, 2002; DOMENÈCH, 2002).

Picture 8 - Implementation favoring landscape and acoustic protection around the Haga Hospital (930 beds), Haia, Netherlands - The Volker Wessels Haga Consortium. Source: http://www.heartbeat5.nl/facilities.asp?Service=Haga%20Hospital&ID=4, 2014.
The architect and researcher Francesc Daumal i Domènech, from University of Cataluña, Spain, defends the relevance of planting trees in the surroundings of hospital building as an important promoter of acoustic comfort since "just by hiding the vehicles physiologically the user of this territory has a weaker perception of the sound waves"(2002, p.157).
An unwelcome sound can be perfectly made milder by the landscape and the results that the density brought by trees can establish as a barrier. Domenèch also highlights that the image of a "naked mountain" reminds the lack of vegetal life and, therefore, it's unnecessary to say how much a "very dense greenwood contributes for the true acoustic barrier that perfectly muffles the sound that could invade the territory" (2002, p.157).
The approach on landscape and noise control receives special focus in the technical standards for health facilities in the United Kingdom, Health Technical Memorandum 08- 01: Acoustics, which recommends on item 2 the Acoustic Criteria to which the design must be based concerning the levels of noise taking into consideration the possibility of changes in the environment and its immediate surroundings. The text brings examples such as the possible intense car traffic the place might attract and therefore increasing the level of noises. The project must therefore foresee the acoustic problems and adopt preventive measures able to anticipate the resulting impacts as reasonable and necessary practices towards human comfort (DEPARTMENT OF HEALTH UNITED KINGDOM, 2006, p. 2).

Picture 9 - Recommendations for the opening of doors aiming to protecting and reducing the level of noise in the neighborhood and avoiding contact with noisy environments. Source: DEPARTMENT OF HEALTH UNITED KINGDOM, 2006, p. 12.
The aforementioned official document - Health Technical Memorandum 08-01: Acoustics - also recommends control and caution in the development of the project with simple concerns for areas that demand privacy and silence in the relationship between the health professional and the patient: doctor offices, interview and reception rooms. Some examples of the architectonic solutions recommended are avoiding door opening to noisy areas and designing landscape protections to decrease the level of noises, like shown in Picture 9.
1.4 The music and the comfort
Another important approach refers to using music in healthcare environments. This is not a consensual matter, although there have been important references concerning its usage in areas or environments in which the sound of music may be defined as a choice or strategy. (KARMAN, 2011; FGI, 2010; NORD, 2009; ROBERTSON, 2001; HOSKING, 1999). Nonetheless, there are scientific evidences of innovative and complementary methodologies to the conventional ones that place "music in a multidimensional care perspective" (ARAÚJO, 2013, p. 1319).
Some studies presented by Carpmann and Grant in Design that Cares (1993) and complemented by Romano Del Nord (2012, 2009), Roger Ulrich (2002, 2001), Paul Robertson (2001), Sarah Hosking (1999) and other researchers (ARAÚJO, 2013; PUGGINA, 2009; KARMAN, 2011; BITENCOURT, 2003) recommend using music as "an audio painkiller" above all in order to help relaxation during medical and deontological procedures.
In the last years of the 20th century the Ministry of Health of Brazil established important comfort strategies in the National Humanization Policy and Management in the Sistema Único de Saúde - HumanizaSUS. Among its recommendations for humanized ambiances the noise receives an emphasized approach and the text recommends "using ambiance music in some spaces like the wards and waiting rooms. It's also important to consider the acoustic protection in order to secure privacy and control noise level" (BRASIL, 2010, p. 122).
One way of providing humanization for submitted patients is using music individually with disposable headphones. This solution to comfort patients is recommended by scientific studies and professionals that deal with acoustic comfort. This practice has been shown successful to "control the mood, reduce aggressiveness and depression" because the "process of listening to music affects positively the release of cerebral chemical substances" (ARAÚJO, 2013, p. 1319).
Headphones can also contribute to 'mask conversations', noisy signs like 'beeps' from breathing machines, scintillation counters, vibration and sounds from mechanical equipments and other noises that "terrify the patients during pre-op and in ICUs". Its usage works as an alert presented by the following observation:
"The headphones allow adopting unique criteria for each patient. The criterion for preference is very interesting; however, we must be careful when choosing the rhythm and the lyrics of the songs" (PUGGINA, 2009, p. 29).
- replacing acoustic alarms with visual ones;
- creating different alarm categories to distinguish life threatening events from routine occurrences;
- periodic analysis of the acoustic profile in areas where patients and health professionals stay;
- reviewing the acoustic impact of equipments;
- releasing the results of researches on the subject, informing the professional team about the possible hearing, physiologic and emotional effects of high-level noise exposure (PUGGINA, 2009, p. 33).
1.5 Cladding materials: imminent conflict
The strategies to attenuate noises within the hospital environment find an extra difficulty concerning high quality materials to acoustic absorption. The molecular constitution of these materials goes against the demands of hygiene control and consequently against the control of hospital infections since the "traps to capture the sounds serve equally as a highly appreciated shelter for microorganisms" (SERAQUI, 1998, p.101).
Brazilians architects Flávio Bicalho and Regina Barcellos, in the text "Materiais de acabamento em estabelecimentos assistenciais de saúde" (CARVALHO, 2002, p. 47), point to the reverberation of the sounds as a relevant aspect to be observed when choosing the floor for hospital environments. This choice aims to preserve the patients' and other users' comfort, above all in the rooms, ICUs and within the secondary circulation areas, close to patient and exam rooms.
The cladding in vinyl, flexible and heterogeneous or linoleum, available in burlaps, PVC resin compounds, pigments, glass fiber and plastics used for tiles are currently the most recommended materials. According to the aforementioned architects its physic homogeneous characteristics and simple handling "allow good cleaning, since the joints are welded on the spot and stay perfectly integrated to the floor forming a monolithic block with the unbroken baseboard" (CARVALHO, 2002, p. 63).
Published in 2010, the most recent review of the North-American technical Standards for projects and constructions of health facilities, Guidelines for Design and Construction of Hospital and Health Care Facilities, coordinated and produced by The Facility Guidelines Institute - FGI -, edition of 2010, recommends some criteria and observations to implement hospital unities concerned with the noise. Such reference also uses the hierarchy of health establishments considering the impact of noises coming from the outside. (FGI, 2010, p. 37).
Table 1 - Clearance and minimal distance to extreme points from the hospital to the source of noises. Source: FGI, USA, 2010.
| Reference for implementation concerning outside noises | Minimum |
Moderate |
Significant | Extreme |
| Level of average sound intensity (day-night) [dB(A)] | <65 | 65 - 70 | 70 - 75 | >75 |
| Level of average daily sound [dB(A)] | <75 | 75 - 80 | 80 - 85 | >85 |
| Distance to the nearest highway (m) | 330 | 75 - 330 | 18 - 250 | <18 |
| Distance to aircraft runways (m) | 2120 | 1060-2120 | 530-1060 | >530 |
| Distance to the nearest railway system (m) | 450 | 225-450 | 33-225 | <33 |
| Outdoor leisure areas for patients [dB(A)] | 45 | 50 | 55 | 60 |
In the same way Table 2 presents the Project Criteria for Minimum-Maximum Noises Inside Health Facilities1 (FGI, 2010).
Table 2 - Minimum-Maximum Design Criteria for Noises in Interior Spaces (FGI, 2010).
| Type of Environment | NC / RC (N) / NRC | dB(A) |
| Patient rooms | 30 - 40 | 35 - 45 |
| Multiple occupant patient care areas | 35 - 45 | 40 - 50 |
| Intensive Care Unity (NICU) | 25 - 35 | 30 - 40 |
| OR, corridor and public spaces | 35 - 45 | 40 - 50 |
| Testing/Research laboratory, minimal speech | 45 - 55 | 50 - 60 |
| Research laboratory, extensive speech | 40 - 50 | 45- 55 |
| Group teaching Lab | 35 - 45 | 40 - 50 |
| Doctor's offices and exam rooms | 30 - 40 | 35 - 45 |
| Teleconference rooms | 25 (max) | 30 (max) |
| Auditorium and large lecture rooms | 25-30 | 30-35 |
Notes:
1 - The Noise Reduction Coefficient (NRC) or Noise Coefficient (NC) must be used to estimate the average coefficient of sound absorption for each environment according to the estimative in Table 2.
2 - A classification system must be chosen to assess the level of noise for each environment and to evaluate the noises originated by the mechanical systems of the building.
Some specific noises in health facilities are a significant source of discomfort for many patients, being at the same time, a discomfort for the professionals who deal directly with caring activities. Usually there is little control over these noises, causing therefore a situation that offers a rather human discomfort factor within the hospital environment.
Even though the Associação Brasileira de Normas Técnicas (ABNT) and the Brazilian legislation recommend several technical and procedure recommendations establishing conditions of acceptability of noises in health facilities there are still some specifications that are not completely contemplated.
The Brazilian Standards from ABNT, NBR 10151 - Acoustic - evaluating the noise in inhabited areas, aiming the comfort of the community - Procedure, published in June 2003 and that incorporates the Erratum from June 1 2003, is the most up to date set of rules and still doesn't present the necessary specificity to the contemporaneity of the problem concerning health facilities.
Just in Table 3 - Level of Evaluation Criteria NCA for outdoor environments in dB(A) from NBR 10151 the "the conditions required for the evaluation of the acceptability of noise in communities regardless the existence of complaints" are established (ABNT, 2003,p.10).
Table 3 - Level of Evaluation Criteria NCA for outdoor environments in dB(A). Source: ABNT NBR 10151, 2003.
| Type of environment | Day dB(A) | Night dB(A) |
| Strictly residential urban area, hospitals or schools | 30 | 40 |
| Mixed area, mostly residential | 50 | 45 |
| Mixed area mostly commercial and administrative | 60 | 55 |
In the Brazilian Standards from ABNT, NBR 10152 Acoustic - Evaluating the ambiance noise in buildings aiming to the comfort of its users - Procedures, some environments from health facilities and its respective acceptable levels of noise are characterized based on sound levels dB (A) and on the "curves of noise evaluation through which a sound spectrum can be compared allowing an identification of more significant ranges frequency and that need correction" (ABNT, 1992, p.3). These information are shown in Table 4 - Values dB(A) and NC presented bellow.
Table 4 - Values dB(A) and NC. Source: ABNT, NBR 1012, 1992.
| Places | Minimum - aximum dB(A) | Minimum - aximum Nc |
|
Hospitals
|
35-45
40-50
45-55
|
30-40
35-45
40-50
|
|
Schools
|
35-45
40-50
45-55
|
30-40
35-45
40-50
|
Notes:
a) The lower value of the range represents the comfortable sound level, while the higher value represents the acceptable sound level for the objective in matter.
b) Higher levels than the ones established in this Table are considered to bring discomfor
The material with high acoustic absorption that can be applied in hospital facilities concern more directly the need of floor cladding for hospital buildings, especially in areas of hospitalization, circulation, doctor offices and intensive care unities. For the ORs, hemodynamic procedure rooms and delivery rooms the requirements for using conductive protection and the respective grounding must be considered.
The installation of this material - conductive floor - aims to reducing the electrostatic discharge that may hit the patient as well as the professionals working in the place. Besides the risk of explosion, due to the low relative air humidity and the acclimatization system "and where anesthesia or chemical material for cleaning are used, the electrostatic discharges can trigger an explosion or even cause a patient to suffer an electric shock" (BICALHO, 2010, p.80).
Although the cladding material must assume the function of acoustic absorption it must also respect the requirements of asepsis control of surfaces and the respective aspects of infection control. The architect Flávio Bicalho gives an important alert on the matter: "Both critical and semi critical areas must receive cladding material that makes the surface smooth, preferentially monolithic or with the smaller number of slits or fissures. This material must assure the maintenance of its features even after intense usage and frequent cleaning" (2010, p. 67).
For wet areas that don't require acoustic comfort with the presented precision, it can be used cladding with high-resistance material if respected the recommendations of the presenting rate of acoustical absorptive surface compatible with the needs in the Resolution RDC nº 50/2002.
The materials, ceramic or not, when used in critical areas cannot have water absorption rate higher than 4% individually or after applied to the environment, moreover, the grout used for the pieces must also present the same absorption rate. Using cement in any anti-absorbent additive for the grout of ceramic pieces or likewise is forbidden for both the walls and the floors of critical areas (BRASIL, 2002, p.107).
For places where critical procedures take place (ORs, enteral nutrition, chemotherapy, hemodynamic procedures, ICUs, Burn Units and likewise areas) the ceiling "must be continuum, being forbidden to use removable fake lining that can interfere in the asepsis of the environment. In the other areas the removable lining can be used, including for reasons related to the maintenance, considering that in the semi-critical areas the linings are resistant to cleaning process, decontamination and disinfection"(BRASIL, 2002, p. 107).
- Fixed Ceiling - Concrete slab and plaster lining continuum or not.
- Removable Ceiling - there are several material and types: metallic, wood, PVC or lined in PVC, cardboard, pressed cardboard.
We must observe, however, the impact of the sound reverberation that each one of these materials can produce in the environment and respective acoustic discomfort they can cause.
Decisions concerning the architectural design to be adopted specifically for buildings addressing healthcare services can be defined by the following recommendations:
- Choose the appropriate field and consider the environmental aspects that may impact the acoustic comfort;
- Evaluate the impact of natural conditions, terrain, topography and geologic conditions when implementing the building;
- Choose and define the design of the building considering the other buildings in the immediate surroundings;
- Organize and distribute the internal spaces considering flows and functional relationships;
- Establish the space distribution and adequate the internal design of the building;
- Define the solutions that might reduce the noises during construction;
- Define and apply materials that reduce the reverberation and absorption of noises;
- Use and apply constructive details that contribute for a better quality of the acoustic system.
2 Comments
The acoustic problem is priority responsibility of the author of the project, who designs the environment who must consider every aspect that may interfere in the quality of the service or the activity that may be developed there. Hence, defining the shape and the applicability of the cladding material must contemplate solutions that attenuate the impact of the sound as well as avoid noisy equipment installed that may promote eventual acoustic discomfort.
The present work doesn't intend to wear out the subject but to promote new reflections on the relevance of the theme at the same time that intends to qualify healthcare environments.
The experiences and related researches referred to throughout this work aim to, above all, offering new fields of research and possibilities of technical and scientific development for healthcare service facilities.
3 References
ABRAHÃO, Júlia et al. Introdução à ergonomia, da teoria à prática. São Paulo: Ed. Blücher, 2009,240 p.
ARAÚJO, Taise C. et SILVA, Luzia W. S. Música: estratégia cuidativa para pacientes internados em Unidade de Terapia Intensiva. Ver. Enfermagem UFPE, Recife, 7 (5): 1319-2, maio, 2013. DOI:10.5205/reuol.3960-31424-1-SM.0705201309. Retrieved Jul 15 2013.
ASSOCIAÇÃO BRASILEIRA DE NORMAS TÉCNICAS (ABNT). Iluminação de ambientes de trabalho. Parte 1: Interior. ABNT NBR ISSO/CIE 8995-1. Rio de Janeiro, abril 2013, 46 p.
_____. Norma de Desempenho de Edificações, Publicada a nova versão da. In: Imprensa. Rio de Janeiro, 2013, 1 p. Retrieved Feb 25, 2014, from: http://www.abnt.org.br/m5.asp?cod_noticia=1230&cod_pagina=962.
_____. Acústica - Avaliação do ruído em áreas habitadas, visando o conforto da comunidade -Procedimento. NBR 10151. Rio de Janeiro, junho 2003, p. 4.
_____. Níveis de ruído em para conforto acústico. NBR 10152. Rio de Janeiro, junho 1992, 7 p.
_____ . Níveis de ruído para conforto acústico, NBR 10152. Rio de Janeiro, 1987. 4 p.
BERNASCONI, Cristiana. L'acustica nella progettazione architettonica - Analisi dei rumore easpetti tecnologici - applicative, soluzioni, materiali e componenti per l'insonorizzazione degli edifici. Progettare e construire. Milano, Itália: A Regola D'Arte. Il Sole 24 ORE S.p.A, 2001. 203 p.il.
BICALHO, Flávio de C. A Arquitetura e a Engenharia no Controle de Infecções. Rio de Janeiro: Riobooks, 2010, 128 p.: Il.
BITENCOURT, Fábio. Ergonomia e conforto humano: uma visão da arquitetura, engenharia e
design de interiores. Editora Rio Books, Rio de Janeiro, 2011, 195 p.: il. Color.
_____; BARROSO-KRAUSE, Claudia; O Conforto Acústico em ambientes de Saúde: estudos de aplicação em centros obstétricos e centros cirúrgicos. Revista PROPEC-IAB/MG - Arquitetura Hospitalar. Belo Horizonte, MG. N.1. ISBN 85-89132-02-1. setembro, 2004, 10 p., il. Retrieved Sep 13, 2013, from: http://www.iabmg.org.br/revistapropec/artigos/O%20CONFORTO%20ACUSTICO%20EM%20AMBIENTES%20DE%20SAUDE.pdf .
BRASIL. Agência Nacional de Vigilância Sanitária. Núcleo Técnico da Política Nacional de Humanização. Acolhimento nas práticas de produção de saúde / Ministério da Saúde, Secretaria de Atenção à Saúde, Núcleo Técnico da Política Nacional de Humanização. - 2. ed. 5. reimp. - Brasília: Editora do Ministério da Saúde, 2010. 44 p. : il. color. - (Série B. Textos Básicos de Saúde).
_____. Agência Nacional de Vigilância Sanitária. Resolução - RDC nº 50 de 21/02/2002. Regulamento Técnico para planejamento, programação, elaboração e avaliação de projetos físicos de estabelecimentos assistenciais de saúde. Brasília, 2002.129 p.il.
CARPMAN, Janet Reizensteinet GRANT, Myron A. Design that cares: Planning Health Facilities for Patient and Visitors. American Hospital Association Company. 2nd edition. Washington, USA,1993. 310 p.il.
CARVALHO, Antonio Pedro Alves de, Org. Temas de Arquitetura de Estabelecimentos Assistenciais de Saúde. Salvador, Ba: Universidade Federal da Bahia. Faculdade de Arquitetura, 2002. 235 p.il.
DEPARTMENT OF HEALTH UNITED KINGDOM. Specialist services: Health Technical Memorandum 08-01: Acoustics. United Kingdom, 2006, 39 p. Retrieved Feb 17, 2014, from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/144248/HTM_08-01.pdf.
DOMENÈCH, Francesc Daumal. Arquitectura acústica , poética y diseño. 1ª ed. Barcelona: Edicions Upc, 2002. 345 p.il.
FGI - The Facility Guidelines Institute.Guidelines for Design and Construction of Health Carefacilities - 2010 Edition.ASHE (American Society for Healthcare Engineering of the American Hospital Association. Chicago, USA, 2010, 411 p.
GRANDJEAN, Etienne. Manual de Ergonomia. Adaptando o Trabalho ao Homem. Trad. STEIN,João Pedro. 4. ed. Porto Alegre: Editora Artes Médicas Sul Ltda., 1998. 338 p.il.
HOSKING, Sarah et HAGGARD, Liz. Healing the Hospital Environment.Design, Management and Maintenance of Healthcare Premises. E & FN SPON. Taylor and Francis Group. London, 1999,193 p.:il. Color.
IIDA, Itiro. Ergonomia,Projeto e Produção. São Paulo: Editora Edgar Blücher Ltda., 2005. 465 p.il.
KARMAN, Jarbas. Jarbas Karman 1917 - 2008. Manutenção e Segurança Hospitalar Preditivas.São Paulo: Estação Liberdade: IPH, 2011, 437 p.: Il.
NORD, Romano Del et PRETTI, Gabriella. L'umanizzazione degli spazi di cura. Linea Guida.Ministerio Della Salue, Itália. Firenze, Itália, 2012, 347 p.: il, Color.
_____. Lo Stress Ambientale nel Progetto Dell'Ospedale Pediatrico: Indirizzitecnici e suggestioni architettoniche. Milano: Motta architettura, 2006, 360 p.: il, Color.
_____. The Culture for the Future of Healthcare Architecture.Proceedings of 28th International Public Health Seminar. Firenze, Italia: AlineaEditrice, 2009, 359 p.: il.
POPE, Catherine et MAYS, Nicholas. Pesquisa Qualitativa na Atenção à Saúde. trad. Ananyr Porto Fajardo, 2ª Ed. Porto Alegre, Artmed, 2005, 118 p.
PUGGINA, Claudia. Humanização em Terapia Intensiva. In: Enfermagem em UTI: cuidando do paciente crítico, Cap. 12. São Paulo. Ed. Manole, 2009, p. 1-41.
ROTHER, Edna Therezinha. Revisão sistemática x revisão narrativa, Editorial. Acta Paul Enferm, 2007, 20 (2), v e vi p. Retrieved Feb 15, 2014, from: http://www.scielo.br/pdf/ape/v20n2/a01v20n2.pdf.
ROBERTSON, Paul. Music and Health. In Design & Health - The therapeutic Benefits of Design. Editor Alain Dilani, Svenskbyggtjänst, Stockolm, 2001, p. 73-79.
SERAQUI, Michel. Guide de l'Ambulatoire. Concevoir et Realiser l'Unité de Soins Ambulatoires.Paris, França :Editions ENSP, 1998. 171 p.il.
SOUZA, Lea Cristina Lucas de, ALMEIDA, Manuela Guedes de, BRAGANÇA, Luís, et NASCIMENTO, Luís Renato do. Bê-a-bá da Acústica Arquitetônica: ouvindo a Arquitetura. 1ªEdição. L.C.L.de Souza. Bauru, São Paulo, 2003. 149 p.il.
ULRICH, Roger S. Health Benefits of Gardens in Hospitals.Center for Health Systems and Design,Texas, USA. 2002, 10 p. Retrieved May 17, 2014, from: http://www.greenplantsforgreenbuildings.org/attachments/contentmanagers/25/HealthSettingsUlrich.pdf.
_____. Effects of Healthcare Environmental Design on Medical Outcomes. Design & Health - Thetherapeutic Benefits of Design. Editor Alain Dilani, Svenskbyggtjänst, Stockolm, 2001, p. 49-59.
WOODSON, Wesley E., TILLMAN, Barry et TILLMAN, Peggy. Human Factors Design Handbook.2ª ed. USA: McGraw-Hill, Inc., 1992. 846 p.il.
YODER,JC, et al. Hospital Noise Puts Patients at Risk. AJN, Arch Intern Med 2012; Vol. 112, No.4, April, 2012. Vol. 112, No. 4.
Send by e-mail:


